Abstract
Background: Post-transplant lymphoproliferative disorder (PTLD) is a major cause of morbidity in transplantation; however, some PTLD subtypes are curable using anti-CD20 immunotherapy alone or with reduction of immunosuppression (R-ISR). We hypothesized that a comprehensive integrated analysis of the tumor immune microenvironment (TME), virome, genome, transcriptome, and cell-free DNA (cfDNA) could offer biologically and clinically relevant insights into the immunobiology of PTLD.
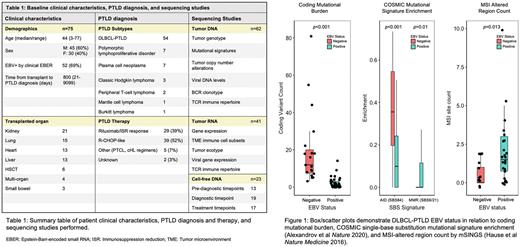
Methods: We identified 75 patients with PTLD after solid organ (n=69) or hematopoietic stem cell (n=6) transplantation. 32 cases occurred <2 years post-transplant (TTD<2, 43%) and 69% were EBV+ by clinical Epstein-Barr-encoded small RNA (EBER) ISH (Table 1). Tumor and cfDNA hybrid capture was performed as previously described, utilizing panels for 322 B-cell lymphoma genes (Kurtz JCO 2018), 180 viral species (Garofalo Blood 2019), and TCR-loci for repertoire profiling (Shukla Blood 2020). Tumor RNAseq was quantified with Salmon & analyzed by DESeq2, fgsea, CIBERSORTx, and Ecotyper.
Results: Tumor microenvironment
Compared to EBV-negative DLBCL-PTLD, EBV+ cases showed significantly higher expression of IFN-associated (MX1, IFI44, IFIT3) and antiviral response genes including CD30/TNFRSF8 and APOBEC3A. TME immune cell subset deconvolution revealed no difference in B-cell populations, but EBV+ cases were enriched in CD4+ memory activated T-cells, M1 macrophages, activated DCs, and eosinophils. Considering lymphoma TME ecotypes (Steen Cancer Cell 2021), the immunoreactive LE4 ecotype identified EBV+ non-GCB cases with median TTD 93 days, while the immune-poor LE8 aligned with EBV- GCB with median TTD 3686 days. TCR repertoires revealed DLBCL-PTLD tumors to have lower T-cell diversity as compared to DLBCL-NOS (p=0.007, Chao1 index), driven by dominant T-cell clones in EBV+ cases.
Virome enrichment by targeted capture confirmed elevated EBV DNA in EBER+ cases, allowing stratification of clinical EBV status by sequencing. While total viral burden and anellovirus level (a marker of immunosuppression) were higher at TTD<2, CMV and HHV6 were similar for later diagnoses.
Mutations & mechanisms
Compared to DLBCL-NOS, DLBCL-PTLD had significantly fewer variants in the NFkB pathway genes MYD88 and PIM1 and several immune regulatory genes (TNFRSF14, B2M, and CD58). In contrast, TP53, CARD11, and TNFAIP3 were similar. Notably, 12 tumors had no detected oncogenic single-nucleotide variants: these cases were all TTD<2 & EBV+. Overall, more coding variants were seen in EBV- PTLD and TTD>2 (p<0.001 for both comparisons) (Fig 1).
We compared mutational signatures within targeted genes to evaluate mechanisms driving these differences. Compared to EBV+ DLBCL-PTLD, EBV- cases were enriched in SBS84, an AID/SHM signature seen in DLBCL-NOS (p<0.001), and had higher AICDA mRNA expression (padj=0.003). Conversely, EBV+ DLBCL-PTLD was enriched in DNA mismatch repair signatures SBS6/21 (p=0.01); and SBS17 (p<0.001), a cryptic mechanism also reported in EBV+ Burkitt lymphomas (Grande Blood 2019). mRNA from EBV+ cases showed corresponding downregulation in the DNA MMR pathway (padj=0.004). Likewise, MSI quantification with mSINGS (Hause Nat Med 2016) showed more altered loci in EBV+ tumors (p=0.013), together suggesting EBV-induced inhibition of MMR as a mutational mechanism.
Clinical response
We compared DLBCL-PTLD patients with complete response to R-ISR to those requiring chemotherapy. Patients with response had shorter TTD but no difference in coding mutation burden. However, the TME of patients requiring chemotherapy contained more M0/non-activated macrophages and regulatory T-cells; similarly, all patients with the immune-depleted TME ecotype LE8 received chemotherapy. While no difference was seen in NFkB pathway genes, patients requiring chemotherapy showed higher expression of MYC & E2F targets.
Conclusions: Through multimodal characterization of the TME and virome in the largest sequencing cohort to date, we identify distinct immunogenomic features reflecting divergent PTLD biology. These include evidence of MMR defects in EBV+ PTLD and TME depletion & MYC pathway enrichment in patients failed by R-ISR, suggesting potential markers of clinical risk. Additional analyses including non-DLBCL cases, viral, and cfDNA data are in progress to further clarify these pathogenetic mechanisms.
Disclosures
Alig:Takeda Pharmaceuticals: Consultancy. Kurtz:Adaptive Biotechnologies: Consultancy; Roche: Consultancy; Genentech: Consultancy; Foresight Diagnostics: Consultancy, Current equity holder in private company, Patents & Royalties. Nijland:Takeda: Research Funding; Roche: Research Funding; Genmab: Consultancy. Andreas:Abbott: Consultancy, Research Funding, Speakers Bureau; Edwards: Consultancy, Research Funding, Speakers Bureau; Medtronic: Consultancy, Research Funding, Speakers Bureau; Boston: Consultancy, Speakers Bureau; Zoll: Consultancy, Speakers Bureau; LSi: Research Funding. Diehn:Foresight Diagnostics: Consultancy, Current equity holder in private company. Khush:CareDX: Membership on an entity's Board of Directors or advisory committees. Alizadeh:Adaptive Biotechnologies: Consultancy; Cibermed Inc: Consultancy, Current equity holder in private company, Patents & Royalties; BMS: Consultancy, Research Funding; Genentech: Consultancy; Karyopharm: Consultancy; Syncopation: Current equity holder in private company, Patents & Royalties; Roche: Consultancy; Gilead: Consultancy, Divested equity in a private or publicly-traded company in the past 24 months, Patents & Royalties; Foresight Diagnostics: Consultancy, Current equity holder in private company, Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal